Squeezing the tube from the middle: why Part B givebacks aren’t always a great fit
Come fall, you’ll be inundated with ads for Medicare Advantage plans, each offering bigger and better benefits than the last. One of the latest...
2 min read
 Action Benefits
:
Nov 3, 2023 11:27:02 AM
Action Benefits
:
Nov 3, 2023 11:27:02 AM

Conventional wisdom tells us it’s beneficial to select a Medicare Advantage plan that each of your doctors participates in. Depending on your plan, out-of-network visits can get very pricy, very quickly. But, this is not one-size-fits-all advice.
There are certain cases where you may actually want to choose a plan where one of your specialists does not participate. Let’s explore the criteria involved in that decision.
Note first: we’re not talking about primary care doctors. As a rule, it’s generally beneficial to select a plan your preferred primary doctor participates in. However, if you’re one of many Americans with a chronic condition, you likely see a specialist at least once a year for monitoring and treatment.
If you see your specialist once per year, with minimal unplanned visits in between, considering plans this doctor doesn’t participate in can vastly expand your options. However, if you see this physician often, choosing a plan that they participate in can save you money.
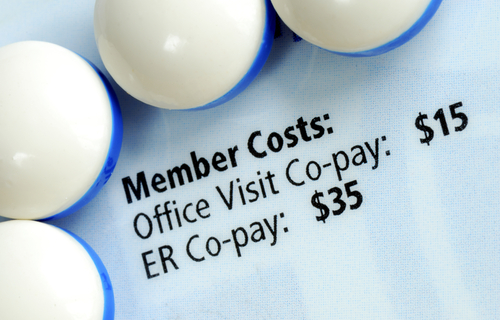
There are two places you’ll see and feel a difference when you visit an out-of-network doctor – your copays, and your Maximum Out Of Pocket spending.
Copays are the flat fees you pay when you see a doctor. They typically increase as you need more complex care. For example, you may pay $0 when you see your primary care physician, but $200 when you visit the Emergency Room.
A common plan design might look like this: you pay $45 dollars when you see an in-network specialist, but $50 when you see an out-of-network specialist. If you’re only spending these five extra dollars once per year, and otherwise enjoy the benefits of your Medicare plan, it could make sense to stay there.
However, if the gap between in-and-out-of-network copays is more significant, it could be a sign to look for a plan that all your doctors take.
The Maximum Out of Pocket limit (MOOP) is the most you’ll pay for care in a plan year. But, this number can be somewhat deceiving. Some plans have separate MOOPs for in-network and out-of-network care, meaning any costs you incur at an out-of-network doctor won’t contribute to your in-network spending limit. In effect, you could have two MOOPs of thousands of dollars each.
However, other plans have a combined in-and-out-of-network MOOP. If you’re considering plans your specialist does not participate with, these types of plans could be a good fit. Any care you get will count toward your single MOOP, leaving you better able to budget for your health care expenses.
If you’re making this decision for the first time, it’s always helpful to have a licensed agent in your corner. Anyone worth their salt can help you run through hypothetical scenarios and see how the costs might pan out for you. Getting assistance from a licensed agent is even more essential if your health needs change, and you begin seeing specialists more frequently. You’ll want to make sure you’re in a plan that effectively balances your health and financial needs – an agent’s specialized quoting tools can help.
Contact our team today for a no-cost benefit consultation. We’ll help you evaluate all your options – even the ones that defy conventional wisdom. Your wallet might be glad you did.

Come fall, you’ll be inundated with ads for Medicare Advantage plans, each offering bigger and better benefits than the last. One of the latest...
Health insurance is helpful in helping you access needed medical care. But, it’s not always easy to understand the variety of payments you might be...

Michigan has one of the most robust health insurance markets in the country. We’re fortunate to have so many high-quality health insurance carriers...